Groin and other abdominal Hernia
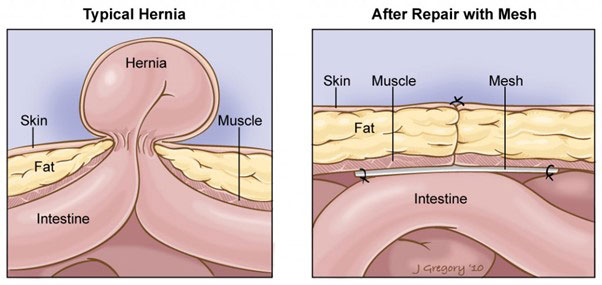
A hernia is when an internal part of the body, often abdominal fat or part of the intestine, pushes through a weakened area in the abdominal wall or groin. Hernias are typically noticed as lumps that become more prominent when standing or straining. Because hernias can contain organs like the intestines, they must be repaired to prevent complications like incarceration or strangulation. A hernia will not heal on its own, and surgical intervention is necessary for proper repair.
What Is Laparoscopic Hernia Repair?
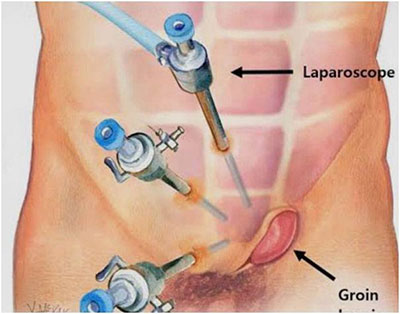
Apart from very small umbilical hernias, most hernias today are repaired using laparoscopic (keyhole) surgery. Mesh reinforcement is considered essential for all but the very smallest of hernias, as it provides additional strength to address the tissue weakness that has led to the hernia in the first place. Mesh design has improved significantly over the past 50 years; modern mesh is strong yet soft, conforms readily to the shape of the abdominal wall, and is macroporous, meaning it has larger spacing between the weave to better allow collagen ingrowth.
The other significant advance has been how the mesh is fixed to the muscle layer- previously titanium tacks were used, which could cause pain if they happened to be positioned close to a nerve. These are now avoided- instead the mesh is held in place with absorbable methods of fixation which dissolve completely within a few weeks. Collagen ingrowth into the weave of the mesh then completes the mesh stabilisation permanently.
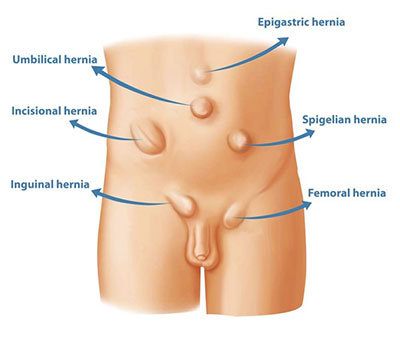
There are two common methods of laparoscopic repair- the TEP (Totally Extraperitoneal) and the TAPP (Trans-abdominal Preperitoneal). The TEP is the preferred technique for groin hernias (inguinal and femoral) whereas TAPP is commonly used for other abdominal hernias (incisional and umbilical). Importantly both methods result in placement of the mesh between the hernia and the lining of the abdominal cavity (the peritoneum), keeping it away from the intestines.
These minimally invasive techniques involve making three small incisions in the abdomen. Through these incisions, a laparoscope (a small camera) is used to view the hernia, whilst 2 laparoscopic grasper instruments then pull the protruding tissue back into place. A suitably sized mesh is then inserted to reinforce the abdominal wall, and over the next 8 weeks, the body grows new collagen tissue into the mesh, securing it in place. Once the mesh is fully integrated, the repair becomes strong and permanent. Local anaesthetic is then infused into the nerves around the hernia repair to provide additional comfort and reduce the need for pain killers.
Benefits of Laparoscopic Hernia Repair
- Minimally invasive: Small incisions mean less tissue disruption, greater precision, less pain, and a quicker recovery.
- Quick recovery: Most patients can go home the same day and return to light activities in 3-7 days.
- No dietary restrictions: You can resume your normal diet immediately after surgery.
- Low complication rate: Laparoscopic surgery has a complication rate of less than 1%.
- Low risk of recurrence: because laparoscopic repairs enable the mesh to be positioned in the ideal plane deep to the muscle layer, behind the hernia, the chance of recurrence is lower than open techniques.
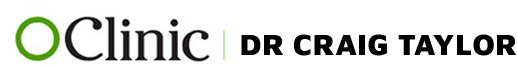
Types of Hernias
Hernias can occur in various parts of the abdomen and groin. Common types include:
1. Inguinal Hernia
Location: Groin area or top of the scrotum.
Presentation: either a lump or discomfort in the groin especially after straining or an episode of heavy lifting.
More common in: Men.
Description: One of the most common types of hernia, often occurring in both children and adults.
Repair: Laparoscopic TEP repair reinforced by mesh.
2. Femoral Hernia
Location: Inner thigh or groin.
More common in: Older adults, particularly women.
Risk: High chance of the hernia becoming incarcerated, requiring immediate repair if it involves the intestine. The method of repair is the same as for inguinal hernias: laparoscopic TEP repair reinforced by mesh.
3. Umbilical & Paraumbilical Hernia
Location: Around the belly button (umbilicus).
Cause: Often due to weakness in the abdominal wall from birth (umbilical) or later in life (paraumbilical).
Repair: Smaller hernias may only need sutures; larger ones require mesh repair via laparoscopy using the TAPP technique.
4. Hiatus Hernia
Location: The diaphragm, where the stomach slides into the chest cavity.
Symptoms: Often causes acid reflux and swallowing difficulties.
Repair: Usually involves a fundoplication procedure using laparoscopic surgery
5. Incisional Hernia
Location: Through an old surgical scar.
Cause: A weakness at the site of a previous surgery.
Repair: Laparoscopic mesh repair (TAPP).
6. Parastomal Hernia
Location: Next to a colostomy or ileostomy.
Symptoms: Can affect the function of the stoma.
Repair: Requires laparoscopic mesh reinforcement.
Risks of Laparoscopic Hernia Repair
While laparoscopic hernia repair is considered safe, there are still some risks:
- General surgical risks: These include bleeding, infection, blood clots, or anaesthesia reactions.
- Specific risks: Mesh infection, ongoing discomfort, and the possibility of the hernia recurring (more common with larger hernias). Recurrences can usually be repaired again using laparoscopic techniques.
Recovery After Laparoscopic Hernia Repair
- Day Surgery: Most patients can go home on the same day, though some may prefer to stay overnight for observation.
- Driving: You can usually drive after 3 days, provided you feel well.
- Return to work: Most people can return to work within 5-7 days, depending on the physical demands of the job.
- Activity restrictions: Avoid strenuous physical activity for 6 weeks to ensure proper healing.